This information was posted during the Medicaid renewal restart period, which ended May 2024.
Your Medicaid will not suddenly end. You will receive communication from the State of Vermont before it is time to provide information to "renew" your coverage.
Medicaid renewal basics
- What is the Medicaid unwind? How long did it last?
- What if I am enrolled in Medicaid for the Aged, Blind, and Disabled (MABD), a Medicare Savings Program (MSP), the Healthy Vermonters Programs (HVP) or VPharm?
- What if my child is enrolled in the Disabled Child Home Care (DCHC) program, also called Katie Beckett Medicaid?
- Will I be contacted about my Medicaid status?
- What kind of communications will I get?
How the Medicaid renewal process could affect you
- When and how do I know when my case will be reviewed?
- What are my options if I can no longer get Medicaid?
- Is anything else about my Medicaid coverage changing?
What Employers need to know
- How does people losing their Medicaid coverage impact my company?
- Can I add an employee or their dependent to my company's health plan?
- Do my employees have health plan options through Vermont Health Connect?
- I don't offer health coverage. What should my employees do?
- Where can I find more information about my obligations under HIPAA?
Medicaid renewal basics
Q: What is the Medicaid unwind? How long did it last?
A: Vermont's renewal process for all Medicaid members began in April 2023. Not all Vermonters enrolled in Medicaid were reviewed for eligibility at the same time. This process happened gradually over the next 12-14 months. Vermonters were contacted ahead of their renewal month.
Q: What if I am enrolled in a different Medicaid program? What if I am enrolled in:
- Medicaid for the Aged, Blind and Disabled (MABD)
- Long-Term Care Medicaid (LTC Medicaid)
- a Medicaid Savings Program (MSP)
- the Healthy Vermonters Programs (HVP), or
- VPharm
A: Just like Medicaid for Children and Adults (MCA) and Dr. Dynasaur, if you were enrolled in one of these programs, you would need to renew your coverage during the unwinding period. We contacted Vermonters when it is time for them to renew. If you or someone in your household was no longer eligible for their current program, you or they would be screened and have a chance to enroll in other coverage.
Q: What if my child is enrolled in the Disabled Child Home Care (DCHC) program, also called Katie Beckett Medicaid?
A: Due to the COVID-19 emergency, Vermont Medicaid stopped most renewals and cut-offs from March 2020 through March 31, 2023. Members who had Disabled Child Home Care (DCHC) kept it during that time. They kept it even if:
- They no longer met the medical or financial rules OR
- They turned 19 years old OR
- They didn't return their Disability Social Report and other information.
Clinical and Financial Reviews
Medical reviews will continue. Financial reviews for this program started again April 1, 2023, and will continue for the next year. These may not happen at the same time. There will be a deadline to return the review forms.
- What if the forms are not returned by the deadline? OR what if the child doesn't meet either the clinical or financial rules? Then the program will end for the child. But first, we will see if they can get another kind of Medicaid.
Q: Will I be contacted about my Medicaid status?
A: Yes. The State of Vermont is committed to supporting Vermonters to maintain some form of health coverage. Your Medicaid won't stop without an opportunity to update your information - including a change in where you live, your household size, or your income. It is important to make sure your mailing address, email address, and phone numbers are correct. Log into your account at www.VermontHealthConnect.gov or call 1-855-899-9600. Long-Term Care (LTC) Medicaid members can contact your specific eligibility specialist to update them directly or call Customer Support at 1-800-250-8427.
We will mail you more when it is your time to renew coverage. It is important that you provide the needed information when you're contacted.
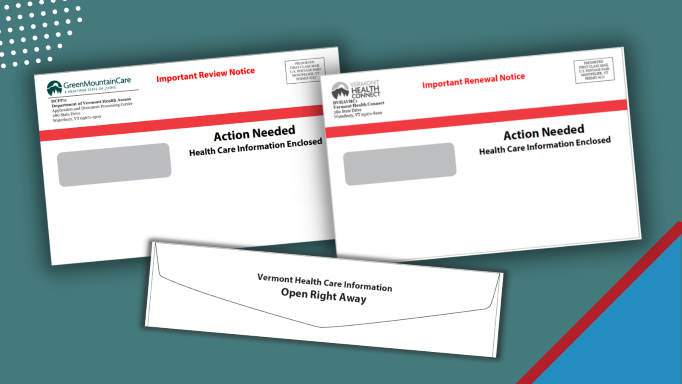
Q: What kind of communication will I get?
A: Your official notice will come in the mail. If you need to take action, your notice may come in an envelope with a red stripe. We may also try to contact you using email, text and by phone if we have that information. Our emails, texts, and calls will never threaten you, or ask you for money or credit card information. They will also never ask you to email or text us back. To learn more about when you can expect your renewal notice, call 1-855-899-9600.
How the Medicaid renewal process could affect you
Q: When and how do I know when my case will be reviewed?
A: When it was your turn to renew, we mailed you more information. Look out for the envelope with the red stripe.
Vermonters received their renewal notices at different times over the unwind period. Most households received a text message or postcard in advance of this mailing.
Q: What are my options if I can no longer get Medicaid?
A: If your Medicaid coverage is going to end because you are no longer eligible, you will get information on how to apply for other health insurance.
Eligible Vermonters can enroll and get help paying for a Qualified Health Plan through Vermont Health Connect. The increased financial help has been extended through 2025. If eligible for Marketplace subsidies, people losing Medicaid coverage may find health plans that, like Medicaid, have zero (or near-zero) monthly premiums.
We urge you to reenroll. To avoid a gap in health coverage, contact us as soon as possible. Learn about more enrollment options.
Q: Is anything else about my Medicaid coverage changing?
A: During the COVID-19 public health emergency, some copays were stopped. Since February 1, 2023, copays for outpatient hospital visits and some drug prescriptions started again. More information about Medicaid copays you can access this link to the Medicaid webpage.
Premiums for Dr, Dynasaur (Medicaid for children under 19 and the pregnant persons) were put on hold during the renewal restart period. NO on lost Dr. Dynasaur coverage if they could not pay during this time.
Have questions? Call Customer Support Center at 1-855-899-9600.
What Employers need to know
Q: How does people losing their Medicaid coverage impact my company?
A: Vermont is again required to see who can get Medicaid. Many people will stay on Vermont Medicaid, but many others will no longer qualify and need new coverage. People who no longer qualify for Vermont Medicaid will get information in the mail. They can also, at any time, go to www.VermontHealthConnect.gov, or call 1-855-899-9600.
Do you have employees who are losing Vermont Medicaid? Now is the time to help them find new coverage. Help ensure they do not have a gap in their health insurance.
- If you DO offer an employer-sponsored group health insurance plan, let employees know about this option right away.
- If you DO NOT offer a group health insurance plan or employees or their dependents are not eligible for the plan, they can find new coverage through Vermont Health Connect.
Q: Can I add an employee or dependent to my company's health plan?
A: Yes. This may be the best an simplest way for your employee and/or their dependents to maintain coverage. If they are found no longer eligible for Medicaid, your employee or their dependent will receive a Medicaid closure notice. This is proof of the loss of coverage. Loss of Medicaid is a qualifying event and allows enrollment in employer health coverage outside of Open Enrollment. Typically, loss of Medicaid provides a 60-day enrollment window, but this can be flexible.
Q: Do my employees have health plan options through Vermont Health Connect?
A: Your employees could choose to explore health coverage options, with financial help, through Vermont Health Connect. Ask them the check the affordability of job-based coverage too.
Q: I don't offer health coverage. What should my employees do?
A: If you have an employee who needs health insurance, encourage the employee to consider coverage through Vermont Health Connect, the state's health insurance marketplace. It offers individuals and families a range of commercials plans that meet state standards for covered essential benefits and services. Signing up with Vermont Health Connects is the only way for your employees to get help paying for health insurance premiums.
Q: Where can I find more information about my obligations under HIPAA?
A: Find more information on HIPAA (the Health Insurance Portability and Accountability Act) requirements for employer-sponsored insurance by using online resources to answer common benefit questions:
- FAQs on Portability and Nondiscrimination Requirements for Workers
- Employee Benefits Security Administration assistance webpage
OR calling the Employee Benefits Security Administration at 1-866-444-3272.
