The Department of Vermont Health Access (DVHA) Special Investigations Unit (SIU) strives to ensure that Medicaid funds are utilized appropriately through the identification and reduction of Medicaid fraud, waste and abuse. Quality control measures designed to help control rising costs of health care and protect diminishing state resources help protect the integrity of our Medicaid program through the elimination of beneficiary and provider fraud, waste and abuse.
FREQUENTLY ASKED QUESTIONS (FAQs)
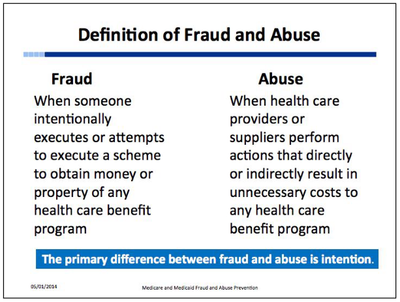
What is Medicaid Fraud? Fraud is intentional deception or misrepresentation that an individual makes knowing it to be false, and may result in unauthorized benefit payments either to that individual or to some other person. It includes any act that constitutes fraud under any applicable federal or state law.
What are some examples of provider or beneficiary fraud?
- Filing claims for services or items not furnished
- Tampering with prescriptions
- Using stolen Medicaid numbers
- Filing claims for visits never made
- Adding charges that don’t exist
- Selling supplies/equipment/medications
- Providing false information
- Medical records
- Claims
- Applications
- Identity of provider or patient
What is Medicaid Abuse? Abuse includes incidents or practices that are not consistent within accepted Medicaid or business standards, and may result in unnecessary costs to Medicaid. Abuse may evolve into fraud.
What are some examples of provider or beneficiary abuse?
- Intentionally underreporting income, assets, resources etc.
- Residing out-of-state
- Drug seeking behaviors
- Over utilization of health care services
- Selling products, medications and/or supplies
- Provider billing irregularities
- Excessive charges for services or supplies
- Claims for services that are not medically necessary
- Improper billing practices by the provider
- Billing for services not provided
- Inaccurate coding
- Misrepresentation of professional credentials/licensing/status of licensure
How do I report suspected Medicaid Fraud, Waste and Abuse?
You may report by using the Health Care Fraud & Abuse Referral Form, or by contacting the DVHA Special Investigations Unit.
